ISSUE1629
- Mark Abramowicz, M.D., President: no disclosure or potential conflict of interest to report
- Jean-Marie Pflomm, Pharm.D., Editor in Chief: no disclosure or potential conflict of interest to report
- Brinda M. Shah, Pharm.D., Consulting Editor: no disclosure or potential conflict of interest to report
- Michael Viscusi, Pharm.D., Associate Editor: no disclosure or potential conflict of interest to report
- Review the efficacy and safety of tocilizumab (Actemra) for treatment of hospitalized patients with COVID-19.
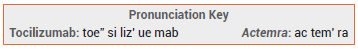
The interleukin-6 (IL-6) receptor antagonist tocilizumab (Actemra – Genentech) has received an Emergency Use Authorization (EUA) from the FDA for IV treatment of COVID-19 in hospitalized patients ≥2 years old who are receiving a systemic corticosteroid and require supplemental oxygen, mechanical ventilation, or extracorporeal membrane oxygenation (ECMO).1 Tocilizumab has been approved by the FDA for various indications, including rheumatoid arthritis and juvenile idiopathic arthritis.
STANDARD TREATMENT — The NIH recommends that patients recently hospitalized (i.e., within the previous 3 days) with COVID-19 who have rapidly increasing oxygen needs, require high-flow oxygen therapy or noninvasive ventilation and have increased markers of inflammation receive the corticosteroid dexamethasone with or without remdesivir, plus either tocilizumab or the oral Janus kinase inhibitor baricitinib (Olumiant). They also recommend that patients with COVID-19 who were admitted to the ICU ≤24 hours previously and require invasive mechanical ventilation or ECMO receive dexamethasone and tocilizumab.2
The Infectious Diseases Society of America recommends use of tocilizumab and a corticosteroid in all hospitalized patients with progressive severe (SpO2 ≤94% on room air) or critical (requiring mechanical ventilation or ECMO) COVID-19 and increased markers of inflammation.3 The WHO recommends use of an IL-6 inhibitor such as tocilizumab and a corticosteroid in all patients with severe or critical COVID-19.4
Use of a corticosteroid such as dexamethasone (off-label) has decreased mortality in patients hospitalized with COVID-19 who require oxygen or ventilation.5 Remdesivir, which is FDA-approved for use in hospitalized patients ≥12 years old who weigh ≥40 kg and available under an EUA for treatment of other hospitalized patients, has shortened the time to recovery in hospitalized adults with COVID-19. Its benefit appears to be greater when given earlier in the illness.6 Baricitinib, which is available under an EUA for the same indication as tocilizumab, has reduced median time to recovery by one day in patients hospitalized for COVID-19 who had radiographic infiltrates, SpO2 ≤94% on room air, or a need for supplemental oxygen or mechanical ventilation.7
MECHANISM OF ACTION — Tocilizumab is a humanized monoclonal antibody that competitively inhibits binding of the proinflammatory cytokine IL-6 to its receptors. In patients with COVID-19, IL-6 inhibition could theoretically prevent development of life-threatening cytokine storm and acute respiratory distress syndrome.8
CLINICAL STUDIES — Issuance of the EUA for tocilizumab was based on the results of four randomized trials in a total of 5606 patients who were hospitalized with COVID-19 pneumonia. Patients received either tocilizumab or placebo in addition to usual care.
The open-label RECOVERY trial included 4116 patients with severe disease. The mortality rate at day 28, the primary endpoint, was significantly lower in the tocilizumab group than in the placebo group (30.7% vs 34.9%; HR 0.85 [95% CI 0.76-0.94]; NNT 24.4). The difference was more pronounced in the prespecified subgroup of patients who were receiving corticosteroids at baseline (29.0% vs 34.9%; HR 0.79 [95% CI 0.70-0.89]; NNT 17.0). Tocilizumab did not decrease mortality compared to placebo in patients who were not receiving corticosteroids at baseline (38.9% vs 34.6%; HR 1.16 [95% CI 0.91-1.48]).9
The double-blind EMPACTA trial included 389 nonventilated patients. Tocilizumab significantly decreased the incidence of the primary endpoint, death or need for mechanical ventilation by day 28, compared to placebo (12.0% vs 19.3%; HR 0.56 [95% CI 0.33-0.97]; NNT 13.7). The drug did not significantly decrease mortality alone (10.4% vs 8.6%) or the median time to discharge or readiness for discharge.10
The double-blind COVACTA trial included 452 patients with severe disease. Compared to placebo, tocilizumab did not significantly improve clinical status at day 28, the primary endpoint, or decrease mortality at day 28 (19.7% vs 19.4%). Median time to discharge or readiness for discharge was significantly shorter with the active drug (20 vs 28 days).11
The double-blind REMDACTA trial (unpublished; summarized in the FDA fact sheet) included 649 patients with severe disease who were also receiving remdesivir. Tocilizumab did not significantly decrease time to discharge or readiness for discharge, the primary endpoint, compared to placebo. It also did not significantly improve mortality or time to mechanical ventilation or death through day 28.12
A prospective meta-analysis included 19 randomized trials that evaluated tocilizumab in patients hospitalized for COVID-19. Addition of tocilizumab to standard care was associated with a significantly lower mortality rate at 28 days compared to addition of placebo (OR 0.83; 95% CI 0.74-0.92).13
ADVERSE EFFECTS — In the clinical trials in patients with COVID-19, serious adverse events occurred more often in patients who received placebo than in those who received tocilizumab.
Serious infections can occur with use of tocilizumab. The drug should not be used for treatment of COVID-19 in patients with other active infections, including localized infections. Neutropenia, thrombocytopenia, serum hepatic transaminase elevations, gastrointestinal perforations, and anaphylaxis have occurred with use of tocilizumab for other indications.
DRUG INTERACTIONS — Use of tocilizumab with other potent immunosuppressants such as baricitinib could result in additive effects and is not recommended. In vitro data indicate that tocilizumab may reverse IL-6-mediated suppression of CYP1A2, 2B6, 2C9, 2C19, 2D6, and 3A4, potentially decreasing serum concentrations of other drugs taken concurrently.
DOSAGE, ADMINISTRATION, AND COST — Actemra is available in single-dose vials containing 80, 200, or 400 mg of tocilizumab. The authorized dose of tocilizumab for treatment of COVID-19 is 12 mg/kg in patients weighing <30 kg and 8 mg/kg in those weighing ≥30 kg (max dose 800 mg). Tocilizumab should be administered as a single IV infusion over 60 minutes. If clinical status does not improve, a second dose can be administered ≥8 hours after the first. The wholesale acquisition cost of one dose of Actemra for a 70-kg patient is $3458.70.14
CONCLUSION — The interleukin-6 inhibitor tocilizumab (Actemra) decreased mortality rates and recovery time in hospitalized patients with COVID-19 who required oxygen or ventilation therapy in some clinical trials, but data supporting its efficacy are mixed. The FDA has authorized use of IV tocilizumab or the oral Janus kinase inhibitor baricitinib (Olumiant) in hospitalized patients ≥2 years old with COVID-19 who are receiving a systemic corticosteroid and require supplemental oxygen, mechanical ventilation, or extracorporeal membrane oxygenation.
- FDA News Release. Coronavirus (COVID-19) update: FDA authorizes drug for treatment of COVID-19. June 24, 2021. Available at: https://bit.ly/3AcipzX. Accessed July 8, 2021.
- NIH. Coronavirus disease 2019 (COVID-19) treatment guidelines. July 8, 2021. Available at: https://bit.ly/3w2faYJ. Accessed July 8, 2021.
- Infectious Diseases Society of America. IDSA guidelines on the treatment and management of patients with COVID-19. June 25, 2021. Available at: https://bit.ly/3xnQqLL. Accessed July 8, 2021.
- WHO. Therapeutics and COVID-19: living guideline. v6.1. July 6, 2021. Available at: https://bit.ly/3wsYsSe. Accessed July 8, 2021.
- RECOVERY Collaborative Group. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med 2021; 384:693.
- Remdesivir (Veklury) for COVID-19. Med Lett Drugs Ther 2020; 62:186.
- An EUA for baricitinib (Olumiant) for COVID-19. Med Lett Drugs Ther 2020; 62:202.
- S Khiali et al. A comprehensive review of tocilizumab in COVID-19 acute respiratory distress syndrome. J Clin Pharmacol 2020; 60:1131.
- RECOVERY Collaborative Group. Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet 2021; 397:1637.
- C Salama et al. Tocilizumab in patients hospitalized with Covid-19 pneumonia. N Engl J Med 2021; 384:20.
- IO Rosas et al. Tocilizumab in hospitalized patients with severe Covid-19 pneumonia. N Engl J Med 2021; 384:1503.
- FDA. Fact sheet for health care providers. Emergency Use Authorization for Actemra (tocilizumab). June 2021. Available at: https://bit.ly/360BR4Q. Accessed July 8, 2021.
- The WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group. Association between administration of IL-6 antagonists and mortality among patients hospitalized for COVID-19: a meta-analysis. JAMA 2021 July 6 (epub).
- Approximate WAC. WAC = wholesaler acquisition cost or manufacturer’s published price to wholesalers; WAC represents a published catalogue or list price and may not represent an actual transactional price. Source: AnalySource® Monthly. June 5, 2021. Reprinted with permission by First Databank, Inc. All rights reserved. ©2021. www.fdbhealth.com/policies/drug-pricing-policy.
