ONLY
ARTICLE
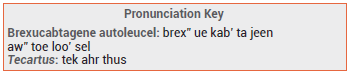
Brexucabtagene autoleucel (Tecartus – Kite) has been approved by the FDA for treatment of adults with relapsed or refractory B-cell precursor acute lymphoblastic leukemia (ALL). It was previously approved for treatment of relapsed or refractory mantle cell lymphoma. Tecartus is an individualized cellular product prepared from the patients own T cells, which are genetically modified to express chimeric antigen receptors (CAR) and then infused back into the patient. The CAR T-cell immunotherapy tisagenlecleucel (Kymriah) was approved in 2017 for treatment of relapsed or refractory B-cell precursor ALL in patients ≤25 years old.1
THE PROCEDURE — Brexucabtagene autoleucel is prepared from autologous T cells obtained by leukapheresis. The T cells are sent to a commercial laboratory, which genetically modifies them via retroviral transduction to insert an anti-CD19 CAR transgene. Tecartus is supplied in a patient-specific, single-dose infusion bag. Before infusion of the genetically modified T cells, patients usually receive lymphodepleting chemotherapy (cyclophosphamide and fludarabine).
CLINICAL STUDIES — FDA approval of the CD19-directed CAR T-cell therapy for the new indication was based on the results of a single arm trial in 55 adults with relapsed or refractory B-cell precursor ALL. Patients were treated with a conditioning regimen of cyclophosphamide and fludarabine and then with anti-CD19 CAR T cells. After a median followup of 26.8 months, the overall complete remission rate was 71%; the median duration of remission was 14.6 months and median overall survival was 25.4 months.2
ADVERSE EFFECTS — The Tecartus label includes a boxed warning about the risk of cytokine release syndrome (CRS), a common complication of CAR T-cell immunotherapy that can cause hypotension, pulmonary edema, coagulopathy, multiorgan failure and death, and about the risk of neurologic toxicity (CAR T-cell encephalopathic syndrome). In the pivotal clinical trial, CRS occurred in 92% and neurologic toxicity occurred in 87% of patients. CRS has been successfully treated with the IL-6 receptor antagonist tocilizumab (Actemra), with or without corticosteroids.
PREGNANCY AND LACTATION — Brexucabtagene autoleucel has not been studied in pregnant or lactating females and is not recommended for use during pregnancy or while breastfeeding. There are no data on the presence of brexucabtagene autoleucel in human breast milk or its effect on the breastfed infant or milk production.
DOSAGE, ADMINISTRATION, AND COST — For treatment of ALL, cyclophosphamide should be administered once daily for 3 days before and fludarabine one day before the single infusion of 1 x 106 CAR-positive viable T cells/kg (target dose; max 1 x 108 cells) in a ~68-mL suspension. Patients should receive acetaminophen and an antihistamine about 30-60 minutes before infusion of Tecartus. They should be monitored at the treatment facility for 2 weeks after the infusion and stay near the treatment facility for at least 4 weeks. The cost for one dose of Tecartus is $424,000 for the drug alone.3
- Tisagenlecleucel (Kymriah) for ALL. Med Lett Drugs Ther 2017; 59:177.
- BD Shah et al. Two-year follow-up of KTE-X19 in patients with relapsed or refractory adult B-cell acute lymphoblastic leukemia in ZUMA-3 and its contextualization with SCHOLAR-3, an external historical control study. J Hematol Oncol 2022; 15:170. doi:10.1186/s13045-022-01379-0
- Approximate WAC. WAC = wholesaler acquisition cost or manufacturer’s published price to wholesalers; WAC represents a published catalogue or list price and may not represent an actual transactional price. Source: AnalySource® Monthly. June 5, 2023. Reprinted with permission by First Databank, Inc. All rights reserved. ©2023. www.fdbhealth.com/policies/drug-pricing-policy.
