ONLY
ARTICLE
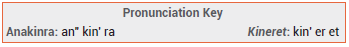
The recombinant interleukin-1 (IL-1) receptor antagonist anakinra (Kineret – Sobi) has been granted an FDA Emergency Use Authorization (EUA) for treatment of hospitalized adults with confirmed COVID-19 pneumonia who require low- or high-flow supplemental oxygen, are at risk of progressing to severe respiratory failure, and are likely to have elevated plasma levels of soluble urokinase plasminogen activator receptor (suPAR).1 Anakinra has been available in the US for years; it is FDA-approved for multiple indications, including rheumatoid arthritis. Assays for suPAR are not commercially available in the US.2
PHARMACOLOGY — Anakinra inhibits IL-1, a proinflammatory cytokine that is associated with lung damage in patients with severe COVID-19. Elevated suPAR levels are associated with increased IL-1 activity, increased rates of respiratory failure and kidney injury, and worse clinical outcomes. Levels of suPAR increase earlier in the course of COVID-19 than levels of other biomarkers such as C-reactive protein and D-dimer.3-5
STANDARD TREATMENT — NIH guidelines state that hospitalized adults with COVID-19 who require conventional oxygen therapy should generally receive the antiviral drug remdesivir (Veklury)6 and the corticosteroid dexamethasone; those with minimal oxygen needs can be treated with remdesivir alone. Patients already receiving dexamethasone who have rapidly increasing oxygen needs should also receive either the Janus kinase inhibitor baricitinib (Olumiant)7 or the IL-6 receptor antagonist tocilizumab (Actemra).8 Those who require high-flow nasal cannula oxygen should receive dexamethasone plus either baricitinib or tocilizumab, with or without remdesivir.9
CLINICAL STUDIES — Issuance of the EUA was based on the results of a double-blind trial (SAVE-MORE) in 594 hospitalized adults with COVID-19 pneumonia (91% had severe disease and required low- or high-flow supplemental oxygen) and elevated suPAR levels (≥6 ng/mL) who were at risk of developing severe respiratory failure. Patients were randomized 2:1 to receive anakinra 100 mg or placebo injected subcutaneously once daily for 10 days, in addition to standard treatment (86% of patients were receiving dexamethasone and 74% were receiving remdesivir).10
At day 28, patients in the anakinra group were significantly less likely than those receiving placebo to have more severe disease as measured by the WHO Clinical Progression ordinal Scale, the primary endpoint (OR 0.37; 95% CI 0.26-0.50). The proportion of patients who experienced severe respiratory failure was also significantly lower in the anakinra group (32.8% vs 21.2%; HR 0.66 [95% CI 0.48-0.92]). The mortality rate was 3.2% with anakinra and 6.9% with placebo (HR 0.48; 95% CI 0.30-1.04).2,10
In two randomized COVID-19 trials that did not select patients based on suPAR levels, one in hospitalized hypoxemic patients who did not require high-flow oxygen or ventilation and the other in patients who required organ support, no significant beneficial effect of anakinra was observed.11,12
ADVERSE EFFECTS — The most common adverse effects of anakinra in SAVE-MORE were increased transaminase levels (31% vs 28% with placebo) and increased gamma-glutamyltransferase levels (14% vs 12%). Neutropenia, serious infections, and hypersensitivity reactions, including anaphylaxis and angioedema, can occur with use of anakinra. The drug is contraindicated for use in patients with hypersensitivity to Escherichia coli-derived proteins.2
PREGNANCY AND LACTATION — Anakinra has not been adequately studied in pregnant women. Administration of supratherapeutic doses of the drug to pregnant rats and rabbits has not been associated with fetal harm. Use of anakinra by breastfeeding women has not been associated with adverse effects.2,13
DRUG INTERACTIONS — Use of anakinra with tumor necrosis factor (TNF) inhibitors can increase the risk of serious infections and is not recommended.
DOSAGE, ADMINISTRATION, AND COST — Anakinra is supplied in 100 mg/0.67 mL prefilled glass syringes. The recommended dosage for treatment of COVID-19 is 100 mg injected subcutaneously once daily for 10 days. In patients with severe renal impairment (CrCl <30 mL/min), a dosage of 100 mg every other day for 10 days (5 total doses) can be considered.2 The wholesale acquisition cost of a 10-day supply of anakinra at the usual dosage is about $1700.14
CONCLUSION — The interleukin-1 inhibitor anakinra (Kineret) improved clinical outcomes more than placebo when added to standard treatment in hospitalized adults with COVID-19 pneumonia who required supplemental oxygen and had elevated levels of soluble urokinase plasminogen activator receptor (suPAR). Assays for suPAR are not commercially available in the US, and anakinra has not been shown to improve outcomes in trials that did not select patients based on suPAR levels. According to the NIH, based on available data and the lack of suPAR assay availability, there is insufficient evidence to recommend for or against use of anakinra in hospitalized adults with COVID-19.15
- FDA News Release. FDA roundup: November 15, 2022. Available at: https://bit.ly/3uhlGMQ. Accessed December 5, 2022.
- FDA. Fact sheet for health care providers: Emergency Use Authorization for Kineret. November 2022. Available at: https://bit.ly/3ETiFXQ. Accessed December 5, 2022.
- H Enocsson et al. Soluble urokinase plasminogen activator receptor (suPAR) independently predicts severity and length of hospitalisation in patients with COVID-19. Front Med (Lausanne) 2021; 8:791716.
- N Rovina et al. Soluble urokinase plasminogen activator receptor (suPAR) as an early predictor of severe respiratory failure in patients with COVID-19 pneumonia. Crit Care 2020; 24:187.
- TU Azam et al. Soluble urokinase receptor (suPAR) in COVID-19-related AKI. J Am Soc Nephrol 2020; 31:2725.
- Remdesivir (Veklury) for COVID-19. Med Lett Drugs Ther 2020; 62:186.
- An EUA for baricitinib (Olumiant) for COVID-19. Med Lett Drugs Ther 2020; 62:202.
- An EUA for tocilizumab (Actemra) for COVID-19. Med Lett Drugs Ther 2021; 63:113.
- NIH. COVID-19 treatment guidelines. Therapeutic management of hospitalized adults with COVID-19. August 8, 2022. Available at: https://bit.ly/3VF47BQ. Accessed December 5, 2022.
- E Kyriazopoulou et al. Early treatment of COVID-19 with anakinra guided by soluble urokinase plasminogen receptor plasma levels: a double-blind, randomized controlled phase 3 trial. Nat Med 2021; 27:1752.
- CORIMUNO-19 Collaborative Group. Effect of anakinra versus usual care in adults in hospital with COVID-19 and mild-to-moderate pneumonia (CORIMUNO-ANA-1): a randomised controlled trial. Lancet Respir Med 2021; 9:295.
- The REMAP-CAP Investigators. Effectiveness of tocilizumab, sarilumab, and anakinra for critically ill patients with COVID-19. The REMAP-CAP COVID-19 immune modulation therapy domain randomized clinical trial. medRxiv 2021 June 25 (preprint). Available at: https://bit.ly/3ue2grY. Accessed December 5, 2022.
- Drugs and Lactation Database (LactMed) [Internet]. Bethesda (MD): National Library of Medicine (US); 2006-. Anakinra. [Updated 2021 May 17]. Available at: https://bit.ly/3AVTuCP. Accessed December 5, 2022.
- Approximate WAC. WAC = wholesaler acquisition cost or manufacturer's published price to wholesalers; WAC represents a published catalogue or list price and may not represent an actual transactional price. Source: AnalySource® Monthly. December 5, 2022. Reprinted with permission by First Databank, Inc. All rights reserved. ©2022. www.fdbhealth.com/policies/drug-pricing-policy.
- NIH. COVID-19 treatment guidelines. Interleukin-1 inhibitors. October 19, 2021. Available at: https://bit.ly/3B2SU66. Accessed December 5, 2022.
